Top 12 Cancer Fighting Supplements of 2024: 1,000+ Studies Analyzed - Part 1
The true story of cancer-fighting supplements is out there. We have compiled and analysed over 1,000 research studies, journal sources, and peer-reviewed papers to uncover the truth.
- Supplement Savvy: Can vitamins and minerals help, or even hinder, cancer prevention?
- Beyond the "Anti-Cancer" Label: This term can be misleading. We'll discuss supplements that may play a role in both prevention and supporting treatment.
These natural diet and supplement strategies can be found in some common, everyday items available in any neighbourhood supermarket.
So why isn’t it making headlines as the greatest cancer breakthrough of the 21st century?
 |
| Credit: FLCCC Alliance |
Cell culture findings carry less weight than results from studies conducted on mice. Similarly, conclusions drawn from mouse studies are surpassed by findings from human studies.
Case studies and preliminary results from small-scale human trials hold less significance than outcomes from umbrella reviews, systematic reviews and meta-analysis*, randomised controlled trials (RCTs), and more extensive, long-term human trials.
- Best Anti Cancer Supplements (Evidence-based)
- Vitamin D3 and K2
- Turmeric (Curcumin)
- Fish Oil (Omega-3 Fatty Acids)
- Vitamin C
- Magnesium and Molecular Hydrogen
- Green tea (EGCG)
- Quercetin
- Melatonin
- Zinc
- Garlic (Allicin)
- Vitamin B2 (riboflavin) and B3 (niacinamide)
- Probiotics
- Can antioxidant supplements help prevent cancer?
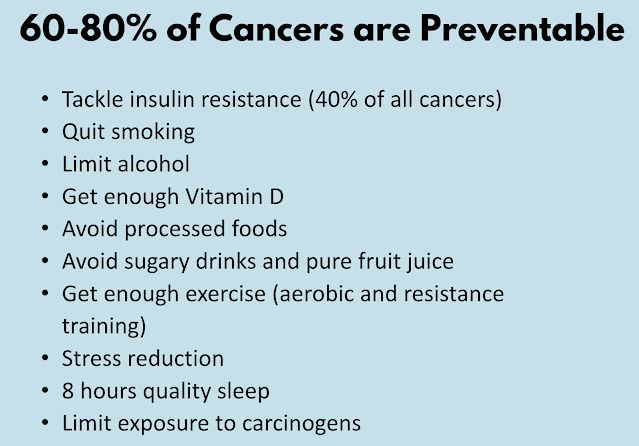
- Causes of Cancer
- Diet and Cancer Prevention
- Don't use tobacco
- Alcohol and Cancer
- Maintain a healthy weight and be physically active
- Fasting and Cancer
- Avoid risky behaviors
- Sleep Quality, Stress and Desk Job
- Protect yourself from the sun
- Get regular medical care and Health Screening
- Avoid unnecessary exposure to radiation.
- Avoid exposure to environmental toxins and infections that contribute to cancer
Best Cancer Fighting Supplements: Evidence Based
1. Vitamin D3 and K2
Vitamin D and Cancer Prevention
Initially researchers believed there was no benefit from taking vitamin D, as they detected no reduced incidence of cancer diagnoses overall. But they were puzzled because cancer deaths went down among those taking the supplements. Meaning, there was no benefit in terms of prevention of cancer but a reduction in cancer deaths was observed.
A secondary analysis, found this anomaly can be explained by the fact that vitamin D seems to stop metastatic cancers - those aggressive types which spread to other parts of the body. That said, when stratified by BMI (body mass index), there was no significant reduction for the vitamin D arm in incident metastatic or fatal cancer among those with overweight or obesity (BMI 25-<30).
The cancers for which the most human data are available are colorectal, breast, prostate, and pancreatic cancer. Numerous epidemiologic studies have shown that higher intake or blood levels of vitamin D are associated with a reduced risk of colorectal cancer (Meta-analysis 2011).
“Vitamin D supplementation is not the magic pill that miraculously solves the cancer burden or that can replace a healthy lifestyle. It is necessary to foster a good environment and invigorate a healthy lifestyle, including a high-quality diet and physical activity. Both have been proven to confer health benefits in many diseases, including cancer, and are the best preventive measures available.”
Research has shown that once you reach a minimum serum vitamin D level of 40 ng/mL (100 nmol/L), your risk for cancer diminishes by 67%, compared to having a level of 20 ng/mL or less.
For health and disease prevention, including cancer prevention, we recommend you aim for optimal levels between 60 ng/mL and 80 ng/mL.
It's important to remember that calcium, vitamin D3, magnesium and vitamin K2 must be properly balanced for optimal overall health. Your best and safest bet is to simply eat more calcium-, magnesium- and vitamin K2-rich foods, along with sensible sun exposure.
However, if you find supplementation is necessary after a serum vitamin D test, also supplement with magnesium and vitamin K2 (MK-7) to ensure proper balance. You'll also want to ensure you're following an overall healthy lifestyle to reduce your cancer risk as much as possible. As researchers explained in Nutrients (2022):
2. Turmeric (Curcumin)
Unfortunately, while there's some curcumin in whole turmeric, there's not enough in the regular spice to achieve clinically relevant results. The turmeric root itself contains only about 3% curcumin concentration. Another major limitation of curcumin as a therapeutic agent is that it is poorly absorbed. When taken in its raw form, you're only absorbing about 1% of the available curcumin.
"Studies on the effect of curcumin on cancer and normal cells will be useful for the ongoing preclinical and clinical investigations on this potential chemo-preventive agent."
3. Fish Oil (Omega-3 Fatty Acids)
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
TOTOX value stands for total oxidation value. The omega 3 fatty acids EPA and DHA from fish oil are highly sensitive to oxidation. This means that they are rapidly affected by contact with oxygen. Oxidised fatty acids are not beneficial to our health. For this reason, a good fish oil supplement has a low TOTOX value. The maximum TOTOX value is set at 26 by the Global Organization for EPA and DHA omega-3.
4. Vitamin C, E and Selenium

There's still no evidence that vitamin C alone can cure cancer, but researchers are studying whether it might boost the effectiveness of other cancer treatments, such as chemotherapy and radiation therapy, or reduce treatment side effects.
There are still no large, controlled clinical trials that have shown a substantial effect of vitamin C on cancer, but some preliminary studies do suggest there may be a benefit to combining standard treatments with high-dose IV vitamin C."
Synthetic Ascorbic acid is NOT the same as whole food or whole fruit vitamin C.
Whole food vitamin C can also boost your copper level, as vitamin C contains an enzyme called tyrosinase, which has 2 atoms of copper in it. Ascorbic acid is prooxidant, while vitamin C complex is actually an antioxidant. Anything that has copper is going to be antioxidant.
5. Magnesium and Molecular Hydrogen
An analysis of the prospective, Swedish Mammography Cohort (JAMA 2005), evaluated 61,433 women aged 40 to 75 without a history of cancer for a mean follow-up of 14.8 years. The highest quintile of magnesium intake was associated with a significantly lower risk of CRC compared with the lowest quintile. This benefit was observed for both colon and rectal cancers.
A case-control study evaluated 2204 subjects from the Tennessee Colorectal Polyp Study (2007), which demonstrated that increasing total magnesium intake was significantly associated with decreasing risk of CR.. The highest tertile of dietary magnesium intake (>298 mg/day) was significantly associated with reduced risk of CRC in an age-adjusted model.
A study of 140,601 postmenopausal women from the Women’s Health Initiative (2015) with an mean follow-up of 13 years demonstrated a significant reduction in CRC risk with the highest quintile of total magnesium intake compared with the lowest quintile of magnesium intake. The benefit was driven by colon cancer, with a trend for rectal cancer.
Magnesium and Pancreatic Cancer
A study of 66,806 subjects aged 50 to 76 at baseline from the Vitamins and Lifestyle cohort (Nature 2015) evaluated magnesium intake and the incidence of pancreatic cancer during a mean follow-up of 6.8 years. Subjects with magnesium intake below the recommended dietary allowance were more likely to develop pancreatic cancer, particularly in those whose intake was less than 75% of the recommended dietary allowance. In this study, a 100 mg/day decrease in magnesium intake resulted in a 24% increase in risk of pancreatic cancer.
6. Melatonin
7. Green Tea (EGCG)
However, the National Center for Complementary and Integrative Health (NCCIH) state that studies of green tea and cancer in humans have so far produced inconsistent results.
8. Quercetin and Cancer
A paper published in August 2022 in Nutrition Research analyzed the pro-apoptotic effect that quercetin has on aging cells. The paper reviewed preclinical and early phase data using quercetin as a senolytic agent and found the data showed it was effective in “preventing or alleviating cancer formation.”
The authors reviewed the importance of cellular aging in the development of cancer cells and the effect that quercetin may have on the suppression of cancer cell proliferation.
Cellular senescence is a dynamic and multi-step process that is associated with alterations in metabolic activity and gene expression. This can compromise tissue regeneration and contribute to aging. On the other hand, by removing senescent cells, age-related dysfunction can be attenuated and potentially extend the lifespan.
9. Zinc and Cancer
10. Garlic (Allicin) and Onion
One study of 543,220 participants found that those who ate lots of Allium vegetables, such as garlic, onions, leeks and shallots, had a lower risk of stomach cancer than those who rarely consumed them (Source).
A study of 471 men showed that a higher intake of garlic was associated with a reduced risk of prostate cancer (Source).
Several clinical studies have found an association between garlic intake and a lower risk of certain types of cancer.
11. Vitamin B2 and B3
Niacinamide at a dose of 50 mg three times per day is a better dose and will provide the fuel for the rate limiting enzyme for NAD+, NAMPT (NicotinAMide PhosphoribosylTransferase). We recommend getting niacinamide in powder form because the lowest available dose in most supplements is 500 mg, and that will decrease NAD+ due to negative feedback on NAMPT, which is the opposite of what you’re looking for.
Other research has shown a beneficial role of niacinamide intake specifically for SCC (squamous cell carcinoma) risk reduction. In one large-scale study involving the Nurses' Health Study and the Health Professionals Follow-up Study, researchers found that total niacin intake was inversely associated with SCC risk. The pooled hazard ratio was 0.84, suggesting a 16% lower risk of SCC for those with higher niacin intake.
12. Probiotics and Gut Microbes
Certain gut bacteria also promote inflammation, which is an underlying factor in virtually all cancers, whereas other bacteria quell it. The presence of certain gut bacteria has even been shown to boost the patient's response to anticancer drugs. (Nature 2018)
One way in which gut bacteria improve the effectiveness of cancer treatment is by activating your immune system and allowing it to function more efficiently. Researchers have actually found that when these specific microbes are absent, certain anticancer drugs may not work at all.
Can Antioxidant Supplements help Prevent Cancer?
To update its 2014 recommendation, the US Preventive Services Task Force (USPSTF) commissioned a review of the evidence on the efficacy of supplementation with single nutrients, functionally related nutrient pairs, or multivitamins for reducing the risk of cardiovascular disease, cancer, and mortality in the general adult population, as well as the harms of supplementation.Many observational studies, including case–control studies and cohort studies, have been conducted to investigate whether the use of dietary antioxidant supplements is associated with reduced risks of cancer in humans. Overall, these studies have yielded mixed results (5). Because observational studies cannot adequately control for biases that might influence study outcomes, the results of any individual observational study must be viewed with caution.
Randomized controlled clinical trials, however, lack most of the biases that limit the reliability of observational studies. Therefore, randomized trials are considered to provide the strongest and most reliable evidence of the benefit and/or harm of a health-related intervention. To date, nine randomized controlled trials of dietary antioxidant supplements for cancer prevention have been conducted worldwide. Many of the trials were sponsored by the National Cancer Institute. The results of these nine trials are summarized here.
It is possible that the lack of benefit in clinical studies can be explained by differences in the effects of the tested antioxidants when they are consumed as purified chemicals as opposed to when they are consumed in foods, which contain complex mixtures of antioxidants, vitamins, and minerals (PubMed 2010).
Causes of Cancer
- sustaining proliferative signaling,
- evading growth suppressors,
- resisting cell death,
- enabling replicative immortality,
- inducing angiogenesis, and
- activating invasion and metastasis.
- deregulating cellular energetics
- avoiding immune destruction
- Genome instability and mutation
- Tumor promoting inflammation
- unlocking phenotypic plasticity,
- non-mutational epigenetic reprogramming,
- polymorphic microbiomes
- senescent cells.
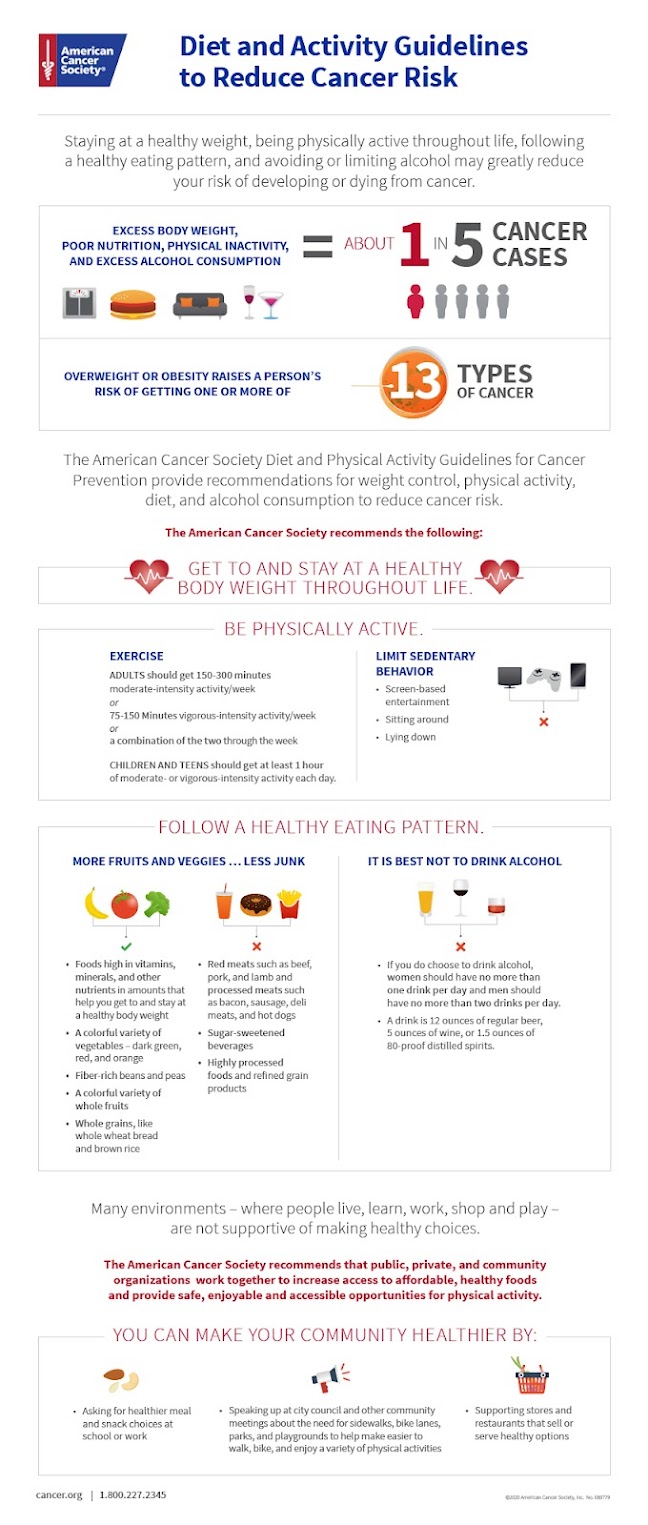
Diet and Cancer Prevention
In 2023, a study published in Cell determined that a ketogenic diet may be an effective nutritional intervention for cancer patients as it helped slow the growth of cancer cells in mice—while a review published in JAMA Oncology in 2022 found that the current evidence available supports a plant-enriched diet for reducing cancer risk.
Intermittent fasting or prolonged fasting refers to periods of restricted calorie intake or complete food avoidance. Like the Ketogenic diet, fasting triggers the use of ketones as the predominant energy source and may sensitize cancer cells to treatments and potentially slow down tumor growth. Fasting-induced metabolic changes may also favor the protection of normal tissues from therapy side effects and improve tolerance and quality of life impacts to care.
- Eat plenty of fruits and vegetables. Basing your diet on fruits, vegetables and other foods from plant sources — such as whole grains and beans. Eat lighter and leaner by choosing fewer high-calorie foods. Limit refined sugars and fat from animal sources.
- Drink alcohol only in moderation, if at all. Alcohol increases the risk of various types of cancer, including cancer of the breast, colon, lung, kidney and liver. Drinking more increases the risk.
- Limit processed meats. Eating processed meat often can slightly increase the risk of certain types of cancer. This news comes from a report from the International Agency for Research on Cancer, the cancer agency of the World Health Organization.
- MIND Diet and Breast Cancer Risk: A 2022 study investigated the association between the MIND diet and breast cancer risk among Tehranian adult women. The study included 134 women with recently diagnosed breast cancer (confirmed histologically) and 272 women of the same age as controls. Results showed that individuals in the highest tertile of the MIND diet had a 45% lower risk of breast cancer compared to those in the lowest tertile.
- Mediterranean Diet and Cancer: The Mediterranean diet is characterized by high consumption of vegetables, fruits, whole grains, and olive oil, while limiting meat, sweets, and saturated fat. Research suggests that the Mediterranean diet is linked to lower risks of cancer and may help alleviate symptoms and imbalances common among people with cancer.
- The abundance of antioxidants and cancer-fighting phytochemicals in this diet contributes to its potential protective effects against cancer (American Institute of Cancer Research 2013).
 |
| Halma et al. 2023 |
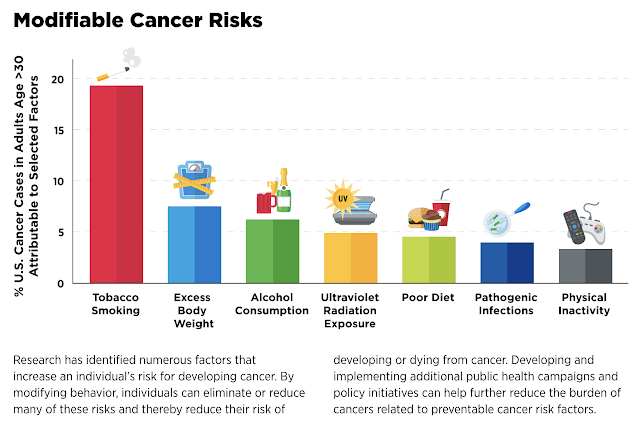
Don't use tobacco
Smoking is a major cause of cancer. Cigarette smoking topped the charts as the leading risk factor, contributing to nearly 20 percent of all cancer cases and close to 30 percent of cancer deaths. Smoking comprised 56 percent of potentially preventable cancers in men and almost 40 percent of those in women. (Journal of the American Cancer Society 2024)But it's not only smoking that's harmful. Chewing tobacco has been linked to cancer of the mouth, throat and pancreas.
Staying away from tobacco — or deciding to stop using it — is an important way to help prevent cancer. For help quitting tobacco, ask a health care provider about stop-smoking products and other ways of quitting.
Maintain a healthy weight and be physically active
Being at a healthy weight might lower the risk of some types of cancer. These include cancer of the breast, prostate, lung, colon and kidney.Physical activity counts too. Besides helping control weight, physical activity on its own might lower the risk of breast cancer and colon cancer.
Doing any amount of physical activity benefits health. But for the most benefit, strive for at least 150 minutes a week of moderate aerobic activity or 75 minutes a week of hard aerobic activity.
You can combine moderate and hard activity. As a general goal, include at least 30 minutes of physical activity in your daily routine. More is better.
“Compared with undertaking no resistance training, undertaking any amount of resistance training reduced the risk of all-cause mortality by 15% ... cardiovascular disease mortality by 19% ... and cancer mortality by 14% ...
A dose-response meta-analysis of 4 studies suggested a nonlinear relationship between resistance training and the risk of all-cause mortality. A maximum risk reduction of 27% was observed at around 60 minutes per week of resistance training ... Mortality risk reductions diminished at higher volumes.”
Fasting and Cancer
Fasting may help reduce obesity-associated cancers. “There’s a lot of obesity-associated cancers,” said Dr. Jason Fung, a nephrologist and fasting expert. “There’s about 13 cancers that are well accepted that they are associated with obesity; fasting might help decrease that.”Fasting can potentially starve cancer cells. When fasting, the body uses fats and produces ketones for energy. Cancer cells rely heavily on glucose, making them less efficient at using ketones.
Additionally, fasting reduces insulin levels. Elevated insulin levels are linked to an increased risk of breast, prostate, and colorectal cancers.
Alcohol
Gut Microbes and Probiotics
Certain gut bacteria also promote inflammation, which is an underlying factor in virtually all cancers, whereas other bacteria quell it. The presence of certain gut bacteria has even been shown to boost the patient's response to anticancer drugs. (Nature 2018)
One way in which gut bacteria improve the effectiveness of cancer treatment is by activating your immune system and allowing it to function more efficiently. Researchers have actually found that when these specific microbes are absent, certain anticancer drugs may not work at all.
Avoid risky behaviors
Another effective cancer prevention tactic is to avoid risky behaviors that can lead to infections that, in turn, might increase the risk of cancer. For example:
Practice safe sex. Limit the number of sexual partners and use a condom. The greater the number of sexual partners in a lifetime, the greater the chances of getting a sexually transmitted infection, such as HIV or HPV.
People who have HIV or AIDS have a higher risk of cancer of the anus, liver and lung. HPV is most often associated with cervical cancer, but it might also increase the risk of cancer of the anus, penis, throat, vulva and vagina.
- Don't share needles. Injecting drugs with shared needles can lead to HIV, as well as hepatitis B and hepatitis C — which can increase the risk of liver cancer. If you're concerned about drug misuse or addiction, seek professional help.
Protect yourself from the sun
Skin cancer is one of the most common kinds of cancer and one of the most preventable. Try these tips:
- Avoid midday sun. Stay out of the sun between 10 a.m. and 4 p.m. when the sun's rays are strongest.
- Stay in the shade. When outdoors, stay in the shade as much as possible. Sunglasses and a broad-brimmed hat help too.
- Cover your skin. Wear clothing that covers as much skin as possible. Wear a head cover and sunglasses. Wear bright or dark colors. They reflect more of the sun's harmful rays than do pastels or bleached cotton.
- Don't skimp on sunscreen. Use a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply a lot of sunscreen. Apply again every two hours, or more often after swimming or sweating.
- Don't use tanning beds or sunlamps. These can do as much harm as sunlight.
Sleep, Stress and Desk Job
The American Cancer Society has also found a link between long periods of inactivity and cancer. The group says that people who spend "prolonged leisure time sitting" — defined as more than 6 hours per day — have a 19% higher rate of death compared to people who sit an average of 3 hours per day. That number includes all causes of death, but it doesn't necessarily mean that sitting directly causes cancer or other diseases, since sick people are also likely to move around less.
Get regular medical care and Health Screening
Doing regular self-exams and having screenings for cancers — such as cancer of the skin, colon, cervix and breast — can raise the chances of finding cancer early. That's when treatment is most likely to succeed. Ask a health care provider about the best cancer screening schedule for you.Avoid unnecessary exposure to radiation.
Get medical imaging studies only when you need them. (Harvard Health)Avoid exposure to environmental toxins and infections that contribute to cancer
Caution and Concern
It's important to emphasize caution when it comes to these natural products. It wasn't long ago that, after finding that people who ate a diet rich in foods containing beta-carotene had a lower risk of lung cancer, researchers set out to study the potential effect of supplements of beta-carotene on risk. Unlike the reduced risk seen with dietary beta-carotene, however, beta-carotene in supplement form was associated with an increased risk of developing the disease.Key Takeaways
- Gendicine, The First Approved p53 Gene Therapy Product for Cancer: 20 Years Track Record
- Best Natural Ways to Anti Aging and Longevity (2024 Edition)





.png)

.png)


.png)

.png)
Comments
Post a Comment